The media has been awash with items about podcasts for dogs and gadgets to monitor dogs that are left on their own for long periods.
The media has been awash with items about podcasts for dogs and gadgets to monitor dogs that are left on their own for long periods.
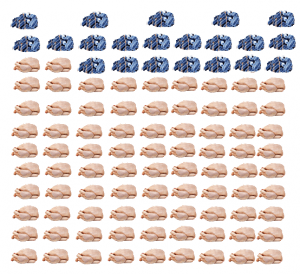
Marketers are aware that pet ownership is big business; more than a quarter of the UK population owns a dog and/or cat and that rises to over half in the US. Mobile telephone ownership has reached saturation point in many parts of the world and automatic upgrading has slowed, so now the emphasis is on selling connectivity to the “internet of things”.
If the thought that all this interconnectivity potentially enables your every movement to be tracked too and that even your refrigerator could be used to spy on your whereabouts, this cannot under any circumstances be the right thing for canine welfare.
No amount of “algorithmically curated playlists” can make up for quality human company for most of the day. No treat dispensing or ball throwing machine can deliver as much fun as an interactive game between dog and human. Dogs will soon habituate to any noise provided for them, even if they pay it any attention in the first place. A dog with true separation disorder is just as likely to tear his nails out trying to dig through the door whether a podcast is playing or not.
If you find yourself considering whether to buy one of these gadgets, work out the purchase price, running and disposal costs and replacement price at end of life and spend the money on buying some training so that you can recall your dog reliably and pay a trainer to provide quality input while you are out. If you contemplate leaving your dog alone all day while you are at work, then please don’t get a dog. You could always volunteer at a rescue at the weekend instead.